Myelomeningocele is a condition in which an infant’s spine does not form normally and the baby is born with a fluid filled sac that is visible outside of the back area. This sac containing a part of the spinal cord, its covering called meninges, and spinal fluid, pushes itself through the space between the spine and the skin. Although there is no exact cause for this disease, lack of folic acid, exposure to viruses or radiation, and genetic factors are suspected causal factors. The babies born with this defect have various difficulties like:
- Weakness and trouble in moving the body parts below the level of the sac
- Poor bowel and bladder control
- Excess spinal fluid in the brain (hydrocephalus)
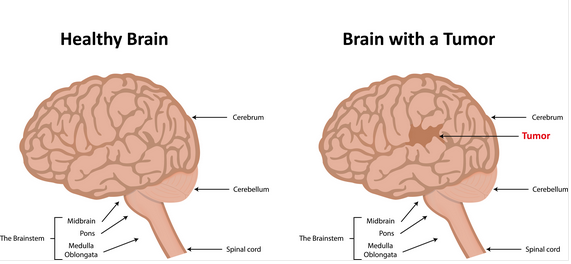
- Malformed brain
- Twisted or abnormal lower limbs
- Impaired cognitive development
- Seizures
A blood test called the quadruple screen during pregnancy can help detect high levels of a protein called alpha fetoprotein (AFP) in your blood which is suggestive that the baby has a higher risk of developing a myelomeningocele. Other tests like ultrasound and amniocentesis can help confirm the diagnosis.
While most cases of myelomeningoceles are surgically repaired soon after birth, some cases of myelomeningoceles are treated with surgery while the baby is in the womb prior to delivery. Surgeries are aimed to correct the deformity, limit the risk of infection and prevent more damage to the spinal cord. At Chennai Brain and Spine, our expert neurosurgeons work together involving multiple specialities to cover your baby’s spinal cord safely within 48 hours of birth.
Visit Us: chennaibrainandspine.com
Mail Us: shyamsundar_krishnan@yahoo.com
Book Appointment: chennaibrainandspine.com/book-appointment.html